Getting candid with Candida
Candida is a fungus that lives on and inside the human body without causing any health problems, however, when the immune system weakens, it turns into a disease causing organism [1]. When it does so, the infection needs to be diagnosed, controlled and treated timely to prevent complications. In this article, we shall talk about the disease-causing yeast and the symptoms of the disease caused by it.
Yeasts are a type of fungi that cause breakdown of sugars and produce various byproducts, some of which may be useful for human consumption [2]. Subsequently, various types of yeasts are used in households and industries to produce consumables like alcohol and bakery products. Some yeasts also live on the human body as harmless microorganisms called commensals. These yeasts live on skin, mouth, gut and genitals and do not cause a disease, unless in very specific circumstances [3,4]. These circumstances may be times when the immune system is compromised, either in extremes of age, or due to some diseases or medicines that cause suppression of the immune system that fights with diseases. At such a time, some of the commensal yeasts turn into disease causing ones [5,6,7]. Even though these disease-causing yeasts cause infections in people with weakened immunity, they may also be responsible for mild infections in normal individuals [8]. However, the severity of infection in the immunocompromised individuals may be greater and so may be the risk of complications.
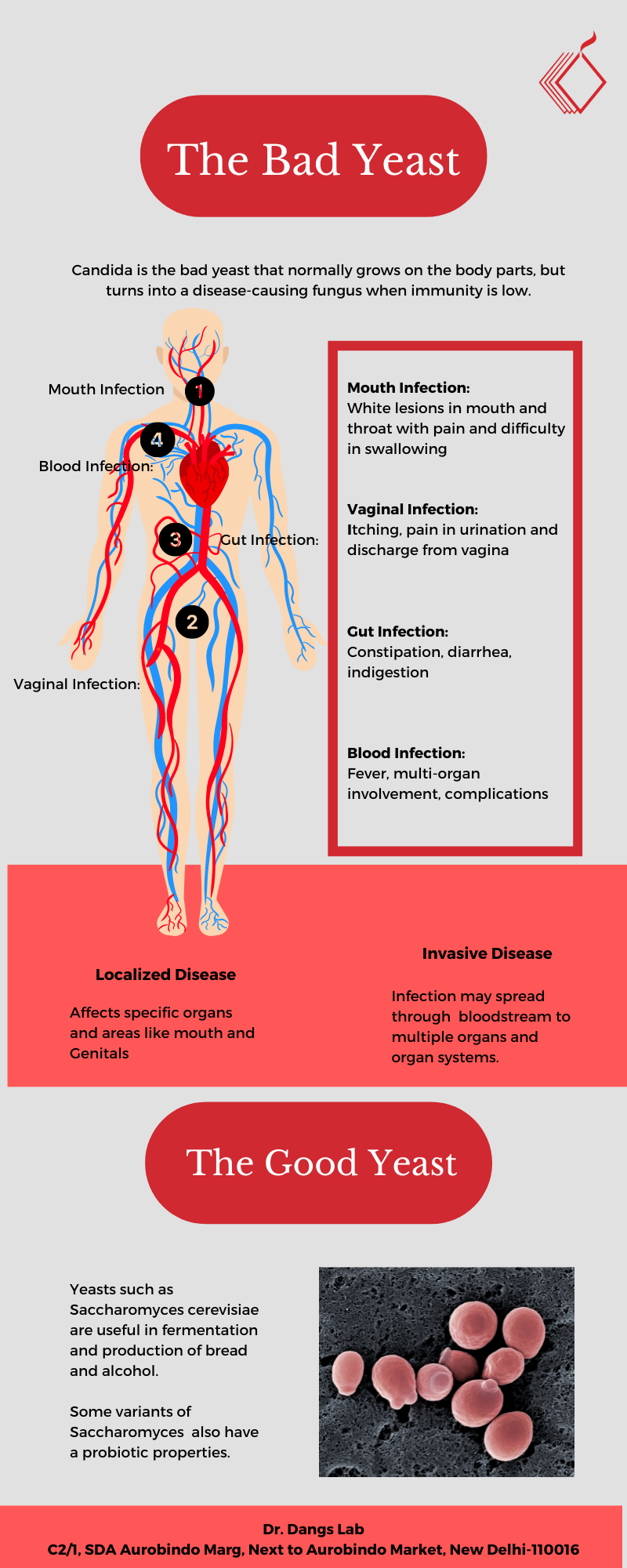
We know yeasts from our kitchens and also know them as important agents in bakery products. Does consuming bakery products also put us at risk of disease? It is not so, say the experts. The yeasts used in bakeries are not the same yeasts as those that cause diseases [9,10, 11] . The bad yeasts are different from the good ones in the functions that certain specific proteins control in their cells. Therefore, even if both the yeasts may look similar, they don't function similarly [10]. Yeasts such as Saccharomyces cerevisiae are used extensively in industry for production of food and beverages especially wines, as well as for biofuel production [12]. Saccharomyces cerevisiae var boulardii is known to act as a probiotic and enhances healthy functioning of the gut [13]. It may help in prevention of diarrhoea and certain gut infections. Such yeasts are different from disease causing yeast. Our gut also normally contains yeasts that are eliminated in stool and may be a part of normal microbial flora. It is therefore not alarming to find certain yeasts in stool.
Yeasts usually infect people with weakened immune systems. Weakened immunity may be due to some diseases or in the extremes of age. Therefore, yeast infections are more common in infants or sometimes in old age. Studies in the US show that about 37% of infants suffer from yeast infection of the mouth [14]. Immunocompromised states from infections such as HIV infections may play an important role in causation of yeast infections.
These infections are usually restricted to a particular body part, which means that they are mostly localized infections. The symptoms usually appear in the mouth and genitals. In the mouth, the yeast infection is commonly known as oral thrush and may present as creamy white lesions with cottage cheese-like appearance which are associated with pain, burning sensation and swelling in the mouth. This may be accompanied with difficulty in chewing and swallowing. In case of genital candidiasis, the symptoms are, itching, pain during urination and intercourse and abnormal vaginal discharge, among other symptoms.
The symptoms are mild in most of the cases, however in immunocompromised conditions, the symptoms may become severe and lead to infection in the bloodstream. In case of such complications, comprehensive management may be required along with hospitalization. These conditions including invasive candidiasis, which may involve multiple organs may lead to serious complications.
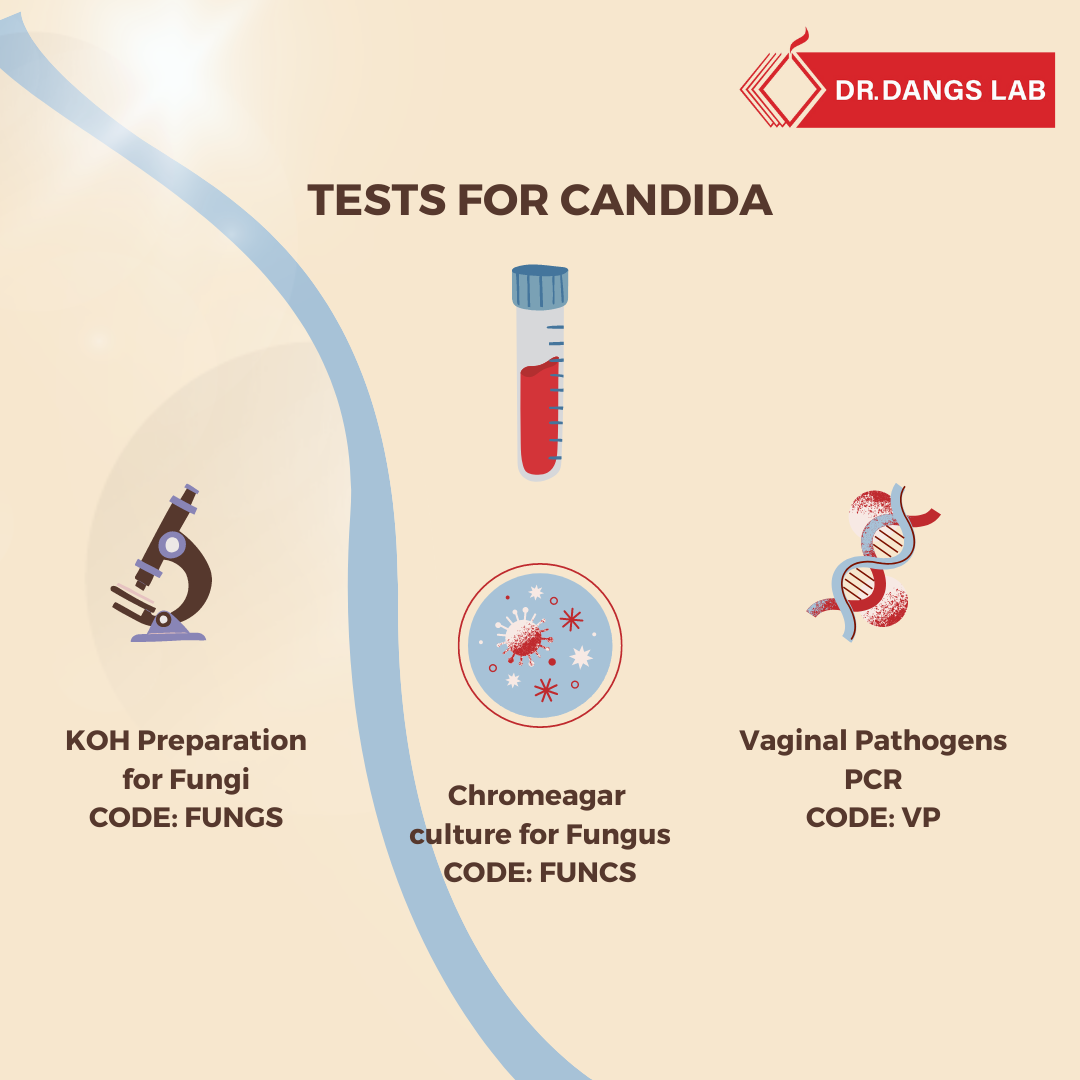
A definitive diagnosis of candidiasis is important for instating the correct treatment. This is done through testing of smear in case of localized infections and blood cultures for infection in blood and multiple organs of the body. The collected samples may be subject to growth on culture medium such as Chromeagar, or to testing through PCR, DNA testing and immunoassays to confirm the presence of infection [15, 16]. Testing and confirmatory diagnosis is important as it is the only way to confirm yeast infection.
Proper mouth and personal hygiene is advisable for prevention of yeast infections. As most of the yeast infections are restricted to certain body parts, maintaining proper personal hygiene may lead to prevention of disease-causing yeast from growing [17]. As yeast infections are usually associated with compromise in the immune system of the body, medications such as steroids that cause immunosuppression may lead to increased susceptibility to yeast infection. Long-term use of steroids or self-medication with steroids without a doctor's prescription should be avoided to prevent any chances of yeast infections. Consuming well cooked and freshly prepared food also reduces any chances of fungal infections. However, if you suspect that you may have a yeast infection, consulting your physician and getting a quick diagnosis may help in early detection and control. You can get more information on yeast you may write to us at (
info@drdangslab.com.)
References